Understanding prostate health is a vital part of every man’s long-term wellness. Over the years, working closely with patients and specialists at Urologic Health Dubai, I have seen one clear pattern: most prostate problems become serious only because they are ignored early on.
This article explains prostate health in simple, practical terms, incorporating the latest insights into the male reproductive system.
Table of Contents
What Is the Prostate and Why It Matters
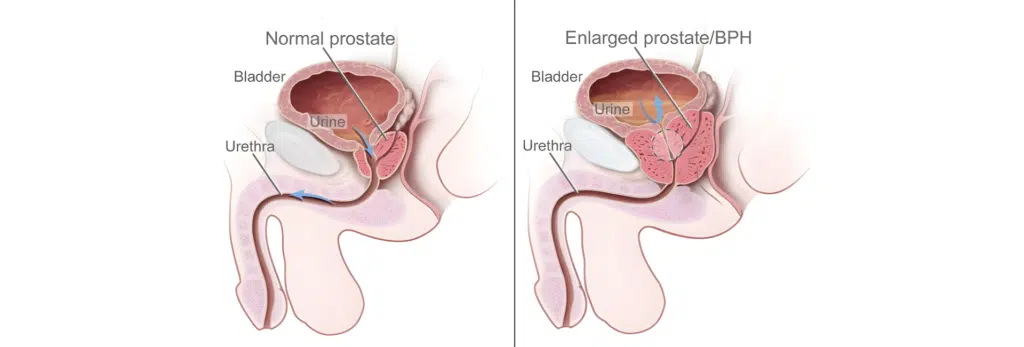
To understand prostate health, it helps to first understand the prostate meaning in real-life terms. The prostate gland is a small, firm, partly muscular organ. It is walnut-sized and located just below the urinary bladder and in front of the rectum. It surrounds a part of the urethra, which is the tube that carries urine and semen out of the body through the penis.
The primary function of the prostate gland is to help make fluid that nourishes and transports sperm cells. This prostatic fluid contains enzymes, zinc, and citric acid – essential components that lubricate the reproductive tract. During orgasm and ejaculation, muscles push these fluids through the urethra as they leave the body.
Anatomy: What does it look like?
The structure of the prostate is complex. It weighs about 1 ounce (roughly 30 grams), which is about as heavy as five U.S. quarters. It is made up of glandular and connective tissues. The gland is divided into five lobes or sections:
- Anterior (in front)
- Posterior (in back)
- Lateral (one on each side)
- Median (in the middle)
The prostatic fascia covers the gland like a sheet of thin, stretchy connective tissue that holds it in place. As men age, the gland usually gets larger; by the time a man is 60, it can grow to the size of a lemon.
Do women have a prostate?
Technically, females don’t have prostates. However, they have Skene’s glands. Some experts believe these glands release a fluid that helps with peeing cleanliness and lubrication during sex. Because they may also release fluid during orgasm like males, some people refer to them as the “female prostate.”
Why Prostate Health Becomes a Concern With Age
Hormonal changes are the primary reason prostate problems mostly affect older men. Testosterone and other hormonal levels shift over time, causing tissues around the gland to become enlarged. This growth is not always dangerous, but because the prostate surrounds the urethra, an enlarged gland can squish the tube. Think of it like a kink in a garden hose – it makes peeing and ejaculating difficult.
Common Prostate Problems in Men
Several conditions can affect the prostate, ranging from benign to severe.
1. Benign Prostatic Hyperplasia (BPH)
BPH is a non-cancerous overgrowth of tissue. It causes the gland to get larger, which may narrow the urethra. This usually happens after age 40. Almost all males develop some enlargement as they age. While isn’t cancer, it can cause blockages and kidney infections if left untreated.
2. Prostatitis
Inflammation or prostatitis occurs when tissues become swollen and tender. It is the most common urinary system issue for men younger than 50. There are four major types:
- Acute bacterial: A sudden infection causing fever, chills, and nausea.
- Chronic bacterial: A recurring infection that lasts several months.
- Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS): The most common but least understood type, causing genital area pain.
- Asymptomatic inflammatory: Doesn’t cause symptoms but shows white blood cells in the semen.
3. Prostate Cancer
Prostate cancer is the second most common type of cancer among men worldwide. It often grows slowly and may not show any initial symptoms. Risk factors include being 50 years older, having a first-degree relative (father, brother, son) with the disease, or inherited gene changes (BRCA1/BRCA2). Race and ethnicity also play a role; it develops more often in African American men, who may experience more aggressive disease.
Symptoms of a “Bad” Prostate
The symptoms depend on the cause, but general conditions usually cause:
- Blood in semen (hematospermia) or blood in pee (hematuria).
- Difficulty starting or stopping urination.
- Weak, slow, or interrupted urine flow.
- Dribbling at the end of passing urine.
- Nocturia: Needing to get up multiple times while sleeping to pee.
- Urgency: Sudden, strong urges to urinate.
- Dysuria: Pain or burning while peeing.
- Dyspareunia: Pain during sexual intercourse.
- Erectile dysfunction: Trouble getting or keeping an erection.
- Loss of bladder control (urinary incontinence).
How Problems Are Diagnosed
A healthcare provider will check your health using several diagnostic tools:
- Digital Rectal Exam (DRE): The doctor inserts a gloved, lubricated finger into the rectum to feel the gland for hard lumps or abnormalities.
- Prostate-Specific Antigen (PSA) Test: A blood test that measures the level of a specific antigen. High levels may indicate BPH, infection, or cancer.
- Urinalysis: Pee tests to provide a sample for signs of bacterial infection.
- Imaging: Transrectal ultrasound or MRI imaging to give a detailed look at suspicious areas.
- Cystoscopy: Uses a pencil-sized, lighted tube with a camera to look inside.
- Biopsy: A needle is used to remove tissue samples to send to a lab for examination.
Practical Prostate Care and Maintenance
While age and genetics are beyond our control, you can promote healthy function through lifestyle choices:
- Eat a Healthy Diet: Include tomatoes (rich in lycopene), cruciferous vegetables (broccoli, cauliflower), and Omega-3 fatty acids (salmon, walnuts). Reduce red meat and processed foods.
- Physical Activity: People who are more active are less likely to have BPH. Aim for 150 minutes of moderate activity per week.
- Hydration: Drink plenty of water to flush out toxins, but limit caffeine and alcohol before bedtime to reduce nighttime urination.
- Quit Tobacco: Smoking is linked to more aggressive cancer risks.
- Regular Screenings: Most males should start discussions with a provider at age 50. Black men or those with a family history may need them earlier (age 40 or 45).
Can You Live Without a Prostate?
Yes. Sometimes providers recommend removing the gland (prostatectomy) to treat cancer. You can live without it, but it may cause side effects such as erectile dysfunction or uncontrollable peeing. These don’t occur in everyone, and advances like robotic surgery have improved outcomes.
Can I feel it myself?
You can’t touch the gland directly from the outside, but you can feel it through the anus or the perineum (the skin between the genitals and anus). A self-exam isn’t as accurate as a DRE by a provider, but many find a prostate massage sexually satisfying. The tissue should feel round, soft, and rubbery, like the tip of your nose. If you feel hard areas or have concerns, talk to a urologist.
Conclusion
Prostate health is an integral part of men’s overall well-being. Understanding the gland’s function and recognizing early signs of disorders empowers you to take charge of your wellness. Whether it is BPH, prostatitis, or cancer, timely medical attention and a proactive lifestyle can make a significant difference in your quality of life.